- ホーム
- 歯の矯正(大阪/吹田)
- Considering whether orthodontic treatment is necessary (adult orthodontics)
Considering whether orthodontic treatment is necessary (adult orthodontics)blog
When forming treatment plans, there is often discussion about whether a patient needs orthodontic treatment.
Here I have collected my own thoughts about full-jaw treatment in particular on deciding if to perform orthodontic treatment.
Please share this if you think it is useful.

I am a general practitioner. I have a neutral view of treatment since I am not a specialist, so I hope this will serve as a reference.
Orthodontics is widely divided into two fields.
1. Occlusal guidance during childhood ・・・There will still be growth of the upper and lower jaw. Occlusal guidance is very important early in this stage.
2. Adult treatment ・・・Growth of the upper and lower jaw is unlikely. There is a low ability to adapt, and acclimation (attrition) with enamel is not likely with a prosthesis. The difficultly increases with complex conditions such as cavities, periodontitis, and tooth loss.
Here we will focus on whether to do adult treatment. (Children do not come to my clinic) There are common purposes between both child and adult treatment, but it can be confusing if talked about at the same time.
For purposes here, we will have to think about any risks with treatment.
When talking about getting treatment, because most people’s teeth has some sort of problem, if a perfect alignment is the standard, then everyone would need treatment.
However, treatment is accompanied by things like a time frame, money, retrogression, pain, and complications. There is a risk of root resorption, gingival recession, and other complications. That is why it is necessary to think about the need for treatment while considering these risks.
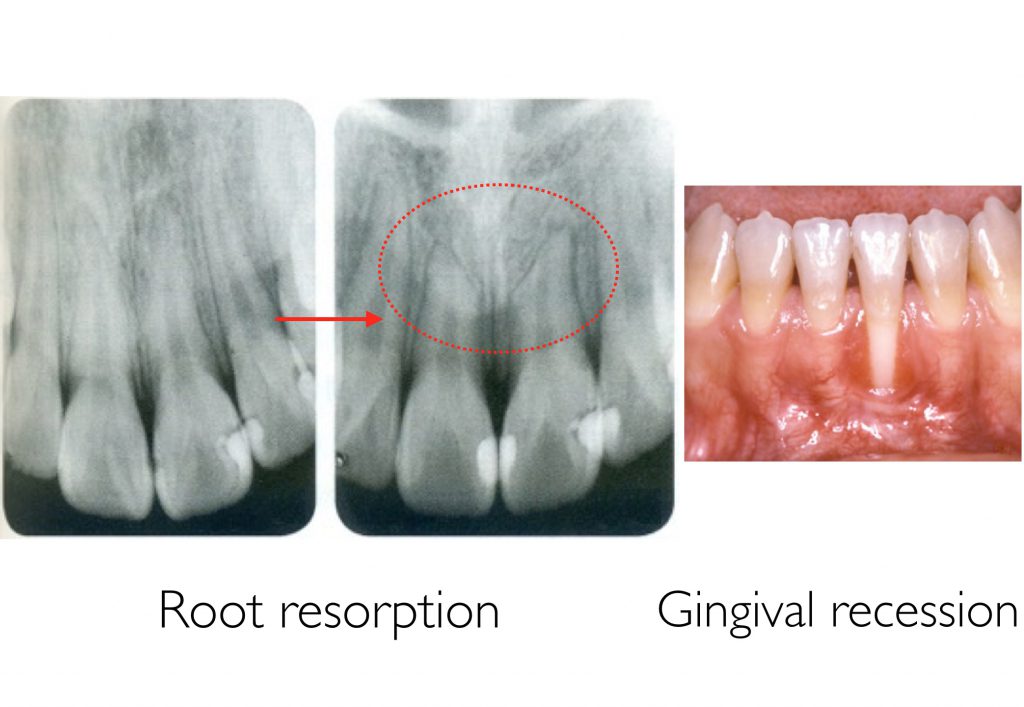
There are many orthodontists who themselves do not get treatment if their teeth are misaligned.
They know that treatment will make their teeth look better, but after thinking about the cost, time frame, pain, retrogression, complications and other risks, they decided themselves whether to have treatment even as orthodontists.
In adult orthodontics, these are the 5 reasons to perform treatment.
1. To improve appearance
2. To improve cleaning
3. To improve eating and chewing
4. To prevent tooth loss due to force
5. Other (per opportunity)
There are many reasons it would be best to perform treatment. I think about the necessity of treatment by comprehensively thinking about all of them. On the other hand, a comprehensive decision in the end would become confusing and mix the issues together. To avoid this, I first categorize the problems. In addition, because there are bound to be multiple problems, I will finally make a decision as a whole.
First is
1. Appearance
Although this is the easiest to grasp, there are a lot of people who do not have a clear understanding.
To begin with, appearance is decided by how the patient feels. Therefore, I think it would be a little strange for an orthodontist to arbitrarily discuss the need for treatment. But because we are professionals, I also think we should make suggestions. For example, if orthodontic treatment would benefit the patient, how different they are numerically from the average person, and what kind of goals they could achieve with treatment with time and money. Even so, the decision is made by the patients themselves.

Most patients come to orthodontists with appearance in mind.
Conversely, general practitioners tend to overlook this important part.
Appearance is broken into two parts: facial, and intraoral.
Facial appearanceis divided into the following:
– Maxillary protrusion (overbite)
– Bimaxillary protrusion (double protrusion)
– Mandibular protrusion (underbite)
Often only intraoral photographs are observed to discuss the need for treatment.
Many general practitioners think about treatment especially in terms of preserving the teeth, and I see cases where there are no photographs that show the facial appearance (particularly from the side) even when consulting patients.

A photograph showing the face is invaluable when discussing whether there should be orthodontic treatment.
For example,

when patients like in the picture above visit, it is not possible to discuss during their examination about the need for orthodontic treatment using only an intraoral photograph.
The appearance is good, the vertical stop (intercuspal position) is stable, and the anterior guidance (molar disclusion) is excellent.
However, if you can see an overbite from the side, you can suggest treatment to improve the appearance.


Although it is sometimes possible to estimate the facial appearance with tooth angles from inside the mouth, it is clear that the appearance is necessary to make a diagnosis.
By the way, the appearance of overbites cannot be improved with tooth straightening alone. If the patient would like their facial appearance to be improved by retracting their lower jaw, orthognathic surgery (osteotomy) is required. (A cephalometric analysis is used to determine the possibility of tooth straightening)

Intraoral appearance
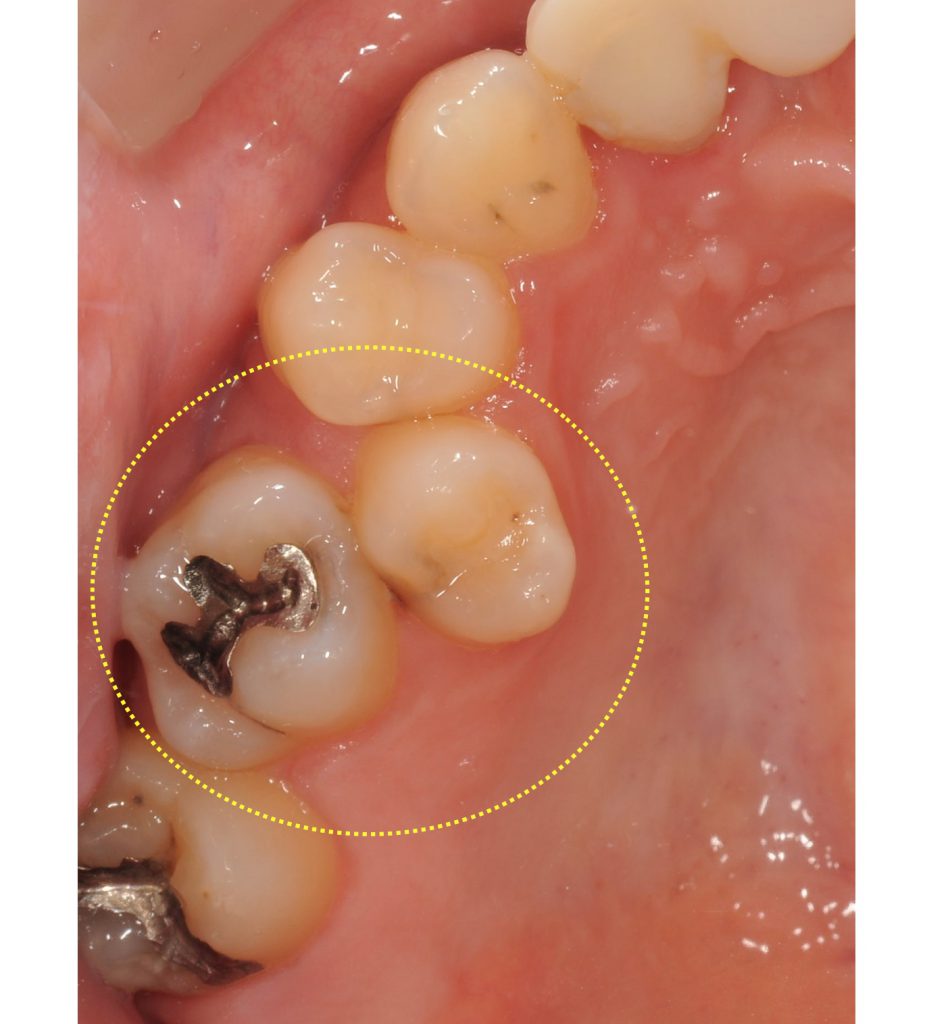
If a patient like in the picture below visits, their facial appearance is perfect.

Nevertheless, you can see a lot of crowding once you look inside their mouth. You must confirm if this bothers the patient.

Think about whether to perform orthodontic treatment to improve appearance while considering these examples.
2. Cleanability


It is common to hear the general public say that it is better to get orthodontic surgery if you have crowded teeth (misalignment) since it is harder to brush them and causes cavities and periodontitis.
It is not a strange thing to recommend treatment to patients with crowding.
But it should also be kept in mind that if they can properly clean their teeth even with crowding, then there is no need for treatment. It is too quick to think about treatment to improve cleanability just from looking intraorally and seeing crowding and built-up plaque.
First, instruct them on proper brushing and flossing techniques. Then, if there are still no improvements, treatment can be recommended.

Of course, cleanability will increase with better alignment if there is crowding, so treatment would be better.
Treatment comes with risks such as cost, time frame, complications, and retrogression, so it becomes necessary to have a basis to recommend treatment as a professional. Certainly, if patients want better tooth alignment with appearance, it would be better to get treatment.
Cleanability may increase with treatment, but you should know if there is a basis to do so.
Would orthodontic treatment help prevent cavities and periodontitis?
– Cavities and orthodontic treatment
According to the systematic review by Hafez et al., it is reported that crowding (misalignment) is not related to cavities.
Hafez HS,Shaarawy SM,AL-Sakiti AA,Mosta YA
Dental crowding as a caries risk factor: a systematic review.2012 Oct;142(4):443-50
http://www.ncbi.nlm.nih.gov/pubmed/22999666
– Periodontal disease and orthodontic treatment
In the systematic review by Bollen et al., there was no reliable evidence that treatment had a positive effect on the health of the periodontal tissue. There is no evidence to use for recommending treatment for preventing periodontitis to the large majority of patients.
Bollen AM1,Cunha-Cruz J,Bakko DW,Huaug GJ,Hujoel PP.J Am Dent Assoc. 2008 Apr;139(4):413-22.
http://www.ncbi.nlm.nih.gov/pubmed/18385025
In short, there is no scientific proof that connects orthodontic treatment with cavity or periodontitis prevention.
But we as dentists know clinically that there are cases where cavities and periodontitis partially progress due to crowding.
Even with no evidence, I do not feel it is wrong to suggest treatment to improve cleanability using a dentist’s discretion.
Also, it must also be remembered that cleanability and be negatively affected by the correction device.
There are cheek-side and tongue-side devices and also mouthpieces. Besides mouthpieces, all other devices must be worn for about 2 to 3 years, and cleanability is worsened.

This means that treatment does not suit patients with bad plaque control. I do, however, absolutely recommend treatment to improve cleanability to highly-motivated patients with good overall plaque control who cannot partially fix their crowding.

I also consider the patient’s cavity risks (pathogens, saliva) and periodontitis risks (pathogens). If the risks are great, crowded teeth can be a problem even with relatively good plaque control.
If performing treatment on patients already with periodontitis, there is quite the risk that it may progress further from the amount of corrective treatment and decline in cleanability. SPR or periodontal surgery must remove tartar beneath the gums, and plaque control fully implemented. Controlling any shifting that occurs after improving teeth alignment must also be taken into account.
First and foremost, after ensuring proper plaque control, decide the need for treatment.

3. Improving eating and chewing

This is the most simple. If patients have a hard time eating from their misaligned teeth and wish to improve it, it would be best to do treatment.
4. To prevent tooth loss due to force
Discussion for this is the most complicated.
When patients come to clinics themselves and ask for treatment, it is mostly to improve appearance. Dentists are the ones who recommend treatment to prevent tooth loss due to force. Dentists have a greater responsibility in their decision-making for this than for appearance.
It is possible to remove strong force with occlusal adjustment (slightly shaving the tooth) or a crown when the force is partial.
It is hard to prove that orthodontic treatment prevents tooth loss due to force, and mostly no scientific evidence as well.
is often used.
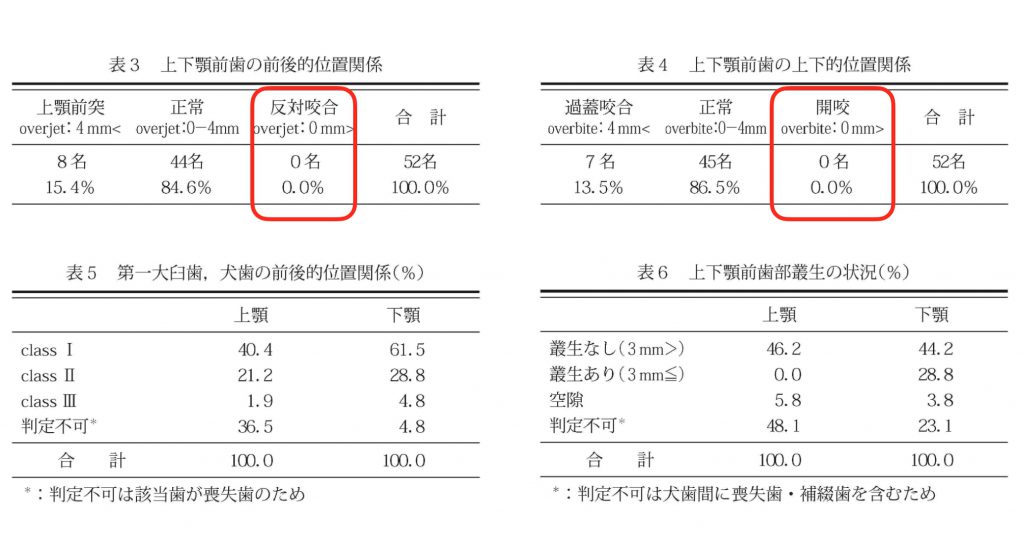
The occlusion of 52 individuals who has achieved the 8020 goal were investigated.
Among them,
84.6% had normal occlusion,
15.4% had maxillary protrusion (overbite),
13.5% had deep overbite (deep occlusion),
0% had reversed occlusion (protruding jaw),
and 0% had an open bite.
The results show that it is rather difficult to have 20 or more teeth over the age of 80 with a protruding jaw or an open bite.
Even the reference work “Observing the occlusion in elderly persons over 80 years old with at least 20 teeth”
shows similar results.
However, supposing we look at these figures, we could also assume that the number of people with reversed occlusion or an open bite were few to begin with. People with reversed occlusion is said to be 4 to 5%. From this, a result of 0% is not something that should cause fear. However, the fact is that there is still a significant difference. (Notwithstanding the sample size for both studies being a little small, with about 50 people)
Even then it is too quick to say that people with a protruding jaw or open mouth need treatment.
If thinking about affects due to strong force, you need to consider their force risks (degree of power). If you decide both the force and power is weak, the need for treatment is low.
I use a force risk diagnostic to investigate the risks of force.
There are greater risks with more prostheses. If natural teeth, there is acclimation due to the wear with enamel.
The basis of diagnosis is vague. It will be greatly influenced by the dentist’s learning environment, held knowledge, skills, and way of thinking.
For determining whether to treat patients orthodontically for occlusal reconstruction,
after considering the facial appearance and prosthetic space and determining the vertical dimension,
take the centric relation bite at that height, and mount the cast in the articulator.
Looking at the anterior coupling of the articular in this state, diagnose whether it is possible to address the problem with only a prosthesis.



When it is possible, if they already have a prosthesis on their maxillary anterior teeth, use only a prosthesis.
When they have many natural teeth, consider using composite resins or laminated veneers, then crowns. After thinking about the risks of grinding, consider treatment without dentures.
While treatment with a prosthesis carries risks such as shaving healthy teeth, damage or loss of teeth, and secondary decay, orthodontic treatment has risks such as time frame, cost, pain, and complications.
Because there are risks for orthodontic treatment and prostheses, I think it is best to use composite resins to address the problem in the least invasive manner.
Even if orthodontic treatment is unnecessary with an anterior coupling diagnosis, there are cases where it is better to have treatment for the facial appearance. In the end, it comes down to a comprehensive diagnosis.
5. Other (per opportunity)
When patients have several missing teeth, even if it is possible to just use implants, sometimes closing the spaces with full-jaw orthodontic treatment has a lower cost. This also improve the facial and intraoral appearance, killing two birds with one stone. Orthodontic treatment is sometimes recommended as the better alternative when looking at cost.
Although must evidence supports implants and they are a wonderful treatment, even they have risks. Scientific risks and not knowing if they will last 30 years. There are risks due to its artificial nature such as peri-implantitis, crown loss, and detachment. Natural teeth is always the best option if possible. Of course, there are risks with orthodontic treatment.
Comprehensively diagnose everything, explain it to the patient, and once you have gained their understanding, have them decide for themselves if they will undergo treatment.
I still have much to learn, but this was my summary of vital clinical points for considering whether orthodontic treatment is necessary for adults.

Thank you very much for reading until the end.
Please share this if you think it is useful.